MEDICINE INTERNSHIP
This is Prateek Pulgurti,a medical student from India. As an intern who worked in the general medicine department, I embarked on a transformative journey, witnessing challenges and complexities of patient care. In this platform, I will share the glimpse into my journey in the department and recount my experiences and lessons I gained during my time in the department.
67 Year old male patient farmer by occupation was brought to the causality with
C/o difficulty in breathing since 20 days
C/o cough with sputum since 20 days
C/o weakness since 20 days
HISTORY OF PRESENT ILLNESS
The patient was apparently asymptomatic 2 years ago, when he developed gradual slowness in movements, gait disturbances and frequent falls.
20 days ago he developed difficulty in breathing which was sudden in onset and progressed gradually from Grade I MMrC to Grade III MMrC, with no diurnal or seasonal variation and no relieving or aggravating factors.
It is also associated with cough, productive, copious amount , white in colours, turbid, thick in consistency , not blood stained and not foul smelling.
H/o sudden fall on his back since 2 years due to loss of postural control.
Falls not associated with any giddiness, vertigo, tiredness, slippage and he was conscious after the fall.
He was taken to a nearby hospital , where a CT scan of the brain was taken and the report showed no abnormalities.
Since the first episode 2 years ago he started developing slowness in all his movements, initially started with the head and neck and has now progressed downwards to affect the lower limbs.
There is no h/o of wasting, thinning of the upper and lower limb muscles
No h/o of difficulty in brushing teeth, buttoning shirts, wearing slippers, getting up from the chair or sitting or sleeping .
He had a history of a similar fall 20 days ago , since which he has developed difficulty in brushing teeth, buttoning shirts, wearing slippers, getting up from the chair, sitting or sleeping .
Movements of the limbs are extremely slow and are not effective in completing any work.
Limbs are stiff and hard
No wasting or thinning
Able to feel clothes, hot and cold sensations
No tingling or numbness reported
No loss or alteration in the consciousness
No speech disturbances.
No delusions, hallucinations, emotional disturbances
No stiffness of neck , fever or vomitings
No h/o diarrhoea , abdominal pain
No h/o palpitations, chest pain
No h/o seizures
PAST HISTORY
K/C/O TB (resolved) underwent treatment 20 years ago
N/K/C/O DM/CAD/CVA/EPILEPSY
K/C/O HTN since 1 year on regular medication
K/C/O Asthma since 6 months and on regular medication
PERSONAL HISTORY
Sleep adequate
Bowel and Bladder - Regular
Appetite - Normal
Habits - Occasional Toddy Drinker
GENERAL EXAMINATION
The patient is conscious, coherent and cooperative
And well oriented to time, place and person
VITALS
Temp - 98.7 F
RR - 34 cpm
PR - 80 bpm
BP - 120/70 mmhg
Spo2 - 93 % on RA
No signs of Pallor, Icterus, Cyanosis, Clubbing or generalised lymphadenopathy
SYSTEMIC EXAMINATION
CVS - S1 S2 Heard, No Murmurs
RS - BAE +
PA - Soft / Non Tender
CNS Examination
The Patient is conscious
Higher Mental Status
Immediate - Intact
Implied - Intact
Long - Intact
GCS - E4V5M6
Right Handed
Neck Rigidity -
Brudzinsky - Negative
Kernig - Negative
Cranial Nerves
1 - intact
2 - intact
3 ,4,6 - Unable to ellicit
5 - Intact
7 - intact
8 - intact
9 - Intact
10 - intact
11 - intact
12 - intact
Joint Position - Intact in both limbs
Stereognosis - Intact in both limbs
Tremors - Intentional, sometimes resting
MOTOR SYSTEM
Right | Left | |
Bulk | Normal | Decreased |
Tone | Hypertonic | Hypertonic |
Power | 4/5 | 4/5 |
Reflexes
Right | Left | |
Biceps | + | + |
Triceps | + | + |
Knee | + | + |
Ankle | + | + |
Plantar | Flexion | Flexion |
OTHER FINDINGS
Slow Occular Saccades +
Gaze Palsy +
Masked Facies +
Serpentine Stare +
Hypophonia +
Bradykinesia +
Rigidity +
Myerson Sign +
CLINICAL IMAGES
PROVISIONAL DIAGNOSIS
PROGRESSIVE SUPRANUCLEAR PALSY (ATYPICAL PARKINSONISM)
[PARKINSON PLUS]
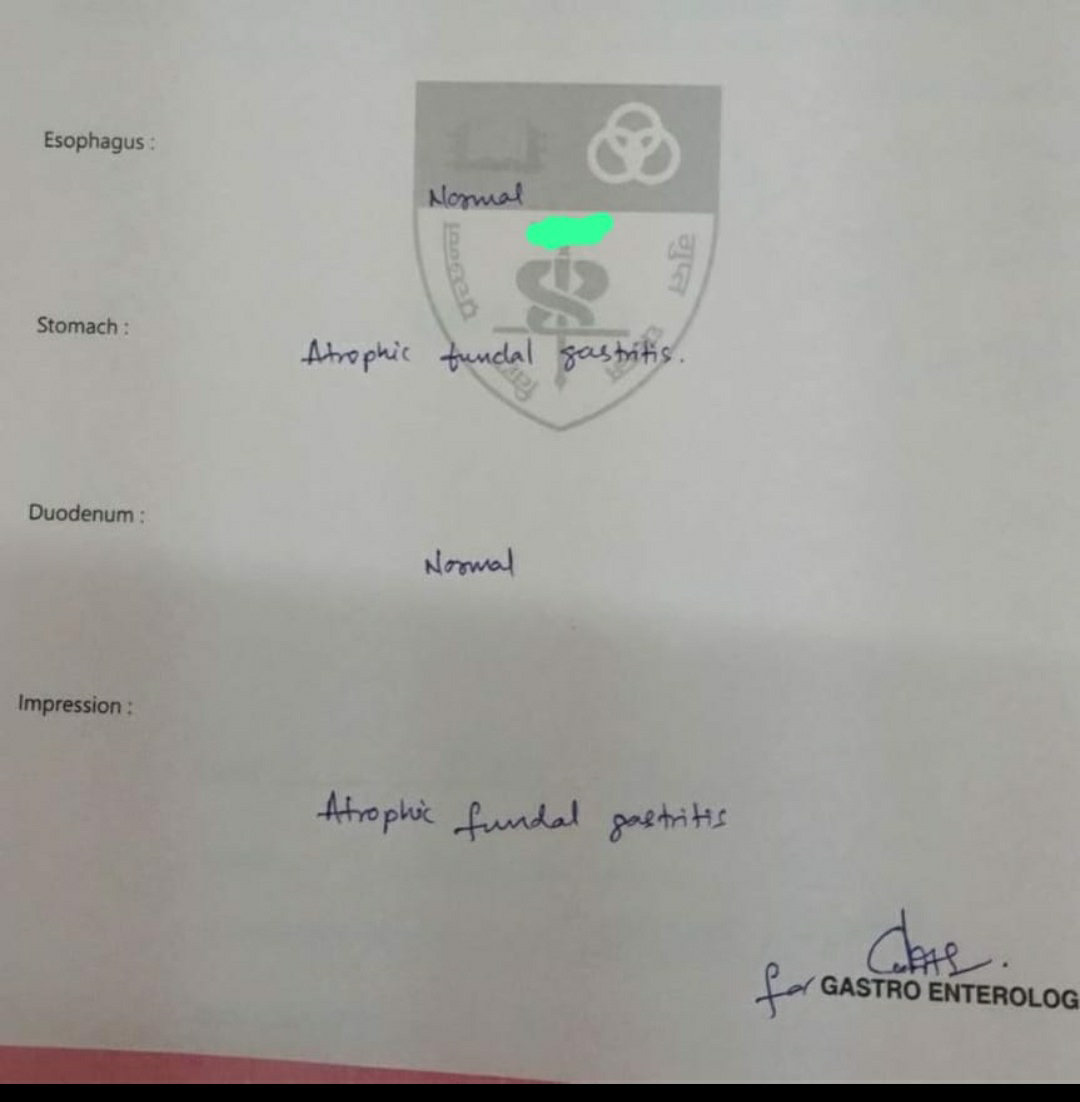
This is a case of 65yr old female ,home maker ,resident of Nalgonda came with c/o abdominal distension since 4 days
- This case made me look into the etiology behind the acid peptic disease.
CASE-3
https://prateekpulgurti127.blogspot.com/2024/01/77m-with-parasthesia-all-over-body.html
- I gained insights into the renal physiology and understood how hemodialysis plays a crucial role in supporting these functions.
- I learnt the importance of patient monitoring during the dialysis sessions including vitals,fluid status and the risk of potential complications.
- I got the opportunity to learn how to acquire the vascular access for hemodialysis.
- I gained the experience in educating the patients about their conditions,the dialysis process and the need for lifestyle modifications with this condition.
CASE-4
This is a case of 35 year old female who came to OPD for the further treatment of her condition as she was already diagnosed as anemic, with the help of my residents we diagnosed that the anemia was secondary to menorrhagia by taking detailed menstrual history.
https://prateekpulgurti127.blogspot.com/2024/01/a-35-year-old-female-with-fever-and.html- The diagnosis of the above case is acute pancreatitis as the serum amylase and serum lipase levels are higher the normal limits.
- In this case,alcohol plays as a significant risk factor for the condition.The excessive alcohol consumption can lead to pancreatic inflammation,contributing to development of this condition.
- The main area of treatment in this particular case is abstinence from alcohol,which is crucial to prevent further damage and reduces the risk of recurrence.
- This case made me look into the causes, classic symptoms,significance of serum markers,treatment strategies associated with the condition.
CASE-6
https://prateekpulgurti127.blogspot.com/2024/01/a-39-year-old-male-with-cough-and-fever.html
- With the help of my post graduates, I learnt the symptoms and signs associated with the various respiratory conditions.
- I got to know how to perform thorough physical examination to identify the clinical conditions and also the importance of imaging studies like x-ray and ultrasound in confirming the presence of such conditions.
 |
| VISUALIZING THE HEART THROUGH A 2D ECHO |
 |
| INSERTING A FOLEYS CATHETER |
 |
| INSERTING A RYLES FEEDING TUBE |
 |
| ASCITIC TAP |
 |
| ABG |
VENIPUNCTURE










Comments
Post a Comment