This
is an online e log book to discuss our patient de-identified health
data shared after taking his / her / guardians signed informed consent.
Here we discuss our individual patients problems through series of
inputs from available global online community of experts with an aim to
solve those patients clinical problem with collective current best
evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome
I
have been given this case to solve in an attempt to understand the
topic of " patient clinical data analysis" to develop my competency in
reading and comprehending clinical data including history, clinical
findings, investigations and come up with diagnosis and treatment plan
The
patient/ attender was informed the purpose of the information being
acquired. An informed consent was taken from patient/ attender and there
is omission of information that was requested to be omitted.
65yr old female ,home maker ,residence of Nalgonda came with c/o abdominal distension and bloating since 4 days
HOPI:
she was apparently asymptomatic 10 days ago then she developed fever
,insidious in onset,low grade ,intermittent type ,not associated with
chills and Rigors ,no aggravating factors,relieving on
medication,associated with body pains.
No h/o burning micturition,headache,cold and cough
C/o
vomitings in these 10 days ,5-6 episode(presently had 1 episode ,with
food particles as content ,non projectile ,non bilious ,non blood
stained
C/o burning sensation in oral cavity since
10days(becoz of which she is unable to eat) ,no h/o dysphagia,loss of
appetite and weight loss
No h/o pain abdomen ,constipation or loose stools
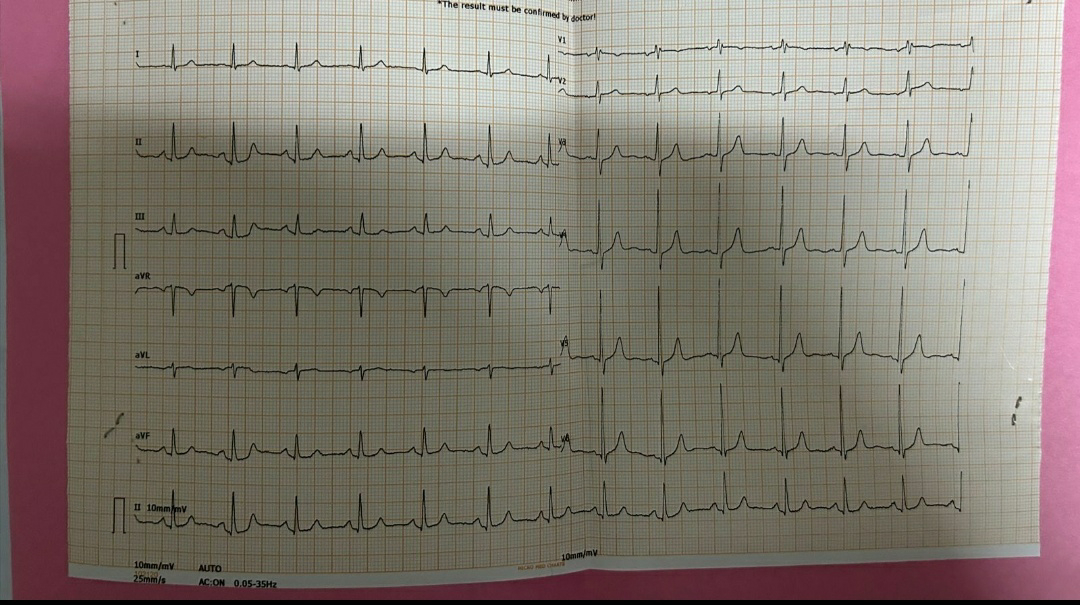
No h/o sob,chest pain ,pedal edema and palpitations and decreased urine output
Now since 4 days c/o abdominal distension with bloating and belching
Associated with regurgitation of food ,aggravating on lying down after taking food and no relieving factors
Past history:
K/c/o DM2 since 6 yrs on regular medication tab.vidagliptin 50mg+metformin 500mg Po/BD
HTN since 6 years on tab telma-H (40-12.5)po/OD
General examination:
Pt is conscious,coherent and cooperative well oriented to time ,place and person
Vitals :
Temp :afebrile
PR:80bpm
RR:16cpm
Grbs:138mg/dl
No pallor ,icterus,clubbing ,cyanosis ,lymphadenopathy,oedema
Systemic examination:
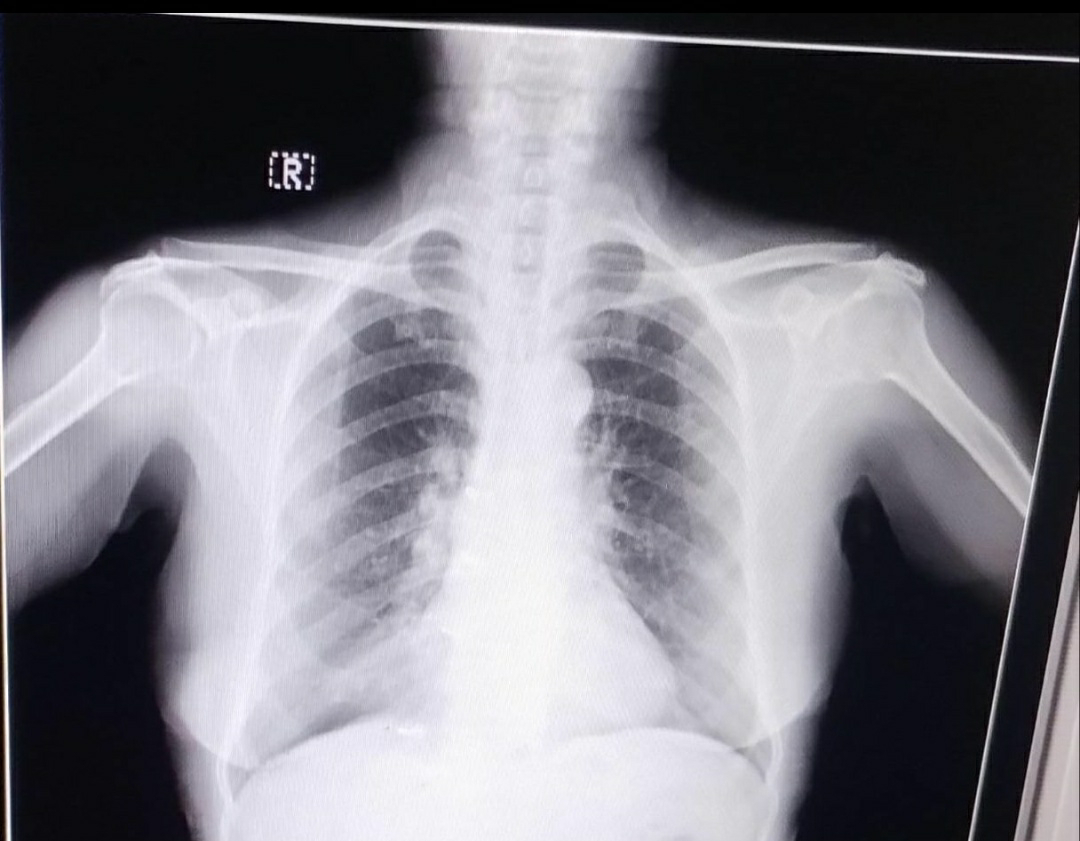
CVS:s1,s2 heard ,no murmurs
RS:BAE+,NVBS +
P/A: distended ,umbilicus :inverted
Non tender ,no organomegaly
No shifting dullness and fluid thrill
Bowel sounds +
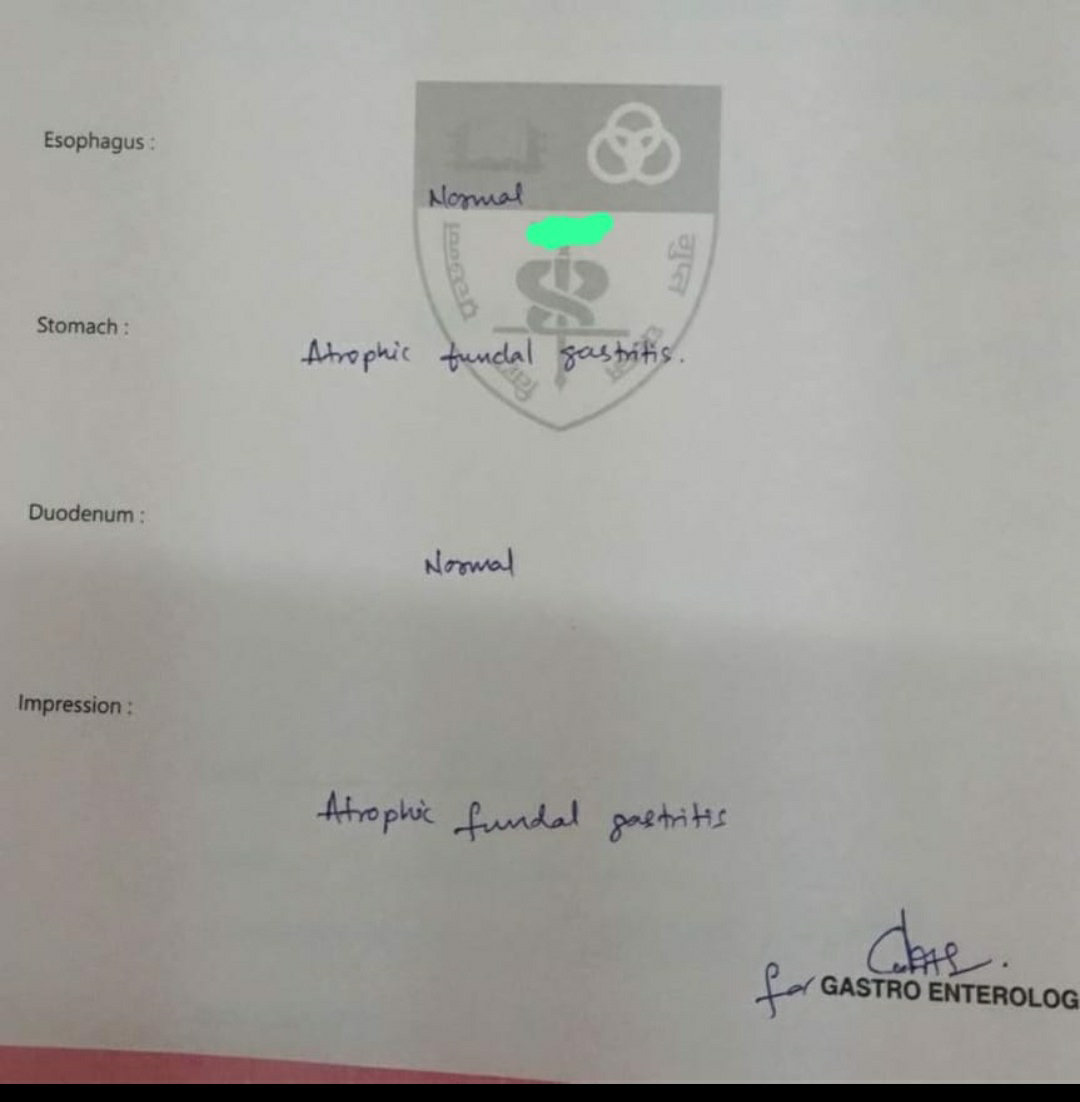
Provisional diagnosis :
GERD under evaluation
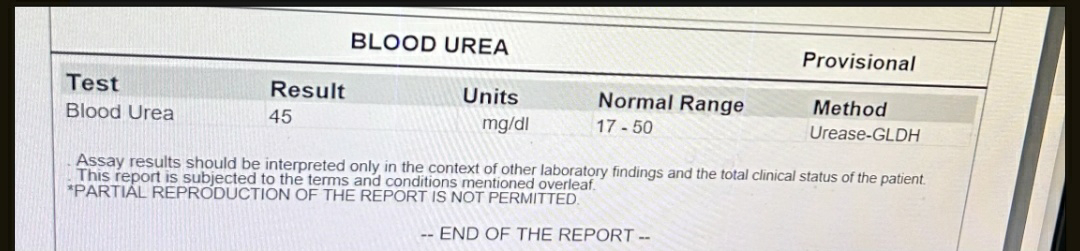
INVESTIGATIONS
HbA1C:6.8%
CUE:
Appearance :clear
Albumin:+
Sugar :nil
Pus and epithelial cells:2-3
RBC:Nil
FINAL DIAGNOSIS:
ACID PEPTIC disease- atrophic gastritis with k/c/o HTN and DM since 6years
CKD:stage 3B
Treatment:
1)tab.RAZO -D 40mg Po/OD before breakfast
2)Syp.sucrafyl-o Po/TID 15mins before food
3)Tab.telma -H 40 po/OD
4)Tab.vidagliptin 50mg+metformin 500mg BD







Comments
Post a Comment