1801006136 - SHORT CASE
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 28 year old female who is a housewife, resident of Miryalguda, came to the OPD with chief complaints of :
- Cough since 1 week
- Shortness of Breath since 1 week
HISTORY OF PRESENTING ILLNESS:
Patient
was apparently asymptomatic 1 week back. Then she developed cough since
1 week which was insidious in onset, gradually progressive, non productive, and aggravated at night.No known relieving factors
She
also complained of breathlessness since 1 week which was insidious in
onset, gradually progressive from mMRC grade II to grade III, associated
with wheeze, palpitations, sweating and Orthopnoea.
C/o chest pain which was dragging type, non radiating on the left side associated with chest tightness, no aggravating or relieving factors .
H/o fever 1 week back, subsided with medication.
On the day of examination the patient complained of productive cough.
There is no h/o loss of appetite, reduced urine output or loss of weight
PAST HISTORY:
No similar complaints in the past
No h/o inhaler usage
No past h/o TB
N/K/C/O HTN, DM, Epilepsy, CAD, asthma
H/o 2 previous LSCS.
PERSONAL HISTORY:
Build and Nourishment : Moderately built, Well Nourished.
Diet: Mixed
Appetite: Normal
Bowel and Bladder: regular
Sleep - Disturbed since last 1 week, was adequate before
No addictions
No known allergies to drugs or food
Daily Routine:
6 AM - Wake up, does morning routine, household chores
9 AM - Prepares breakfast, sends children to school, and husband to work
10 AM - 12 PM - Watches TV
1230 PM - 1 PM - Prepares and has Lunch
2 PM - 4 PM - Takes a nap
4 PM - Socialises with neighbours
5 PM - Children and husband return home, has some tea and snacks
6 PM - 7 PM - Spends time with family
8 PM - Prepares Dinner
9 PM - 10 PM - Has dinner and watches TV
10 PM - Goes to bed
FAMILY HISTORY:
No history of similar complaints in the family
MENSTRUAL HISTORY:
Age of menarche: 12 years.
Cycle: 3/28
Not associated with pain or clots
LMP: 1/12/22
OBSTETRIC HISTORY:
Age of marriage: 18 years
Age at first child birth: 22 yrs
Para: 2
Number of living children:3
Birth history: LSCS
GENERAL EXAMINATION:
The patient is conscious, coherent, cooperative, and well oriented to time, place and person.
No pallor, icterus, cyanosis, clubbing, koilonychia, lymphadenopathy or edema
No malnutrition or dehydration
VITALS:
Temp: Afebrile
PR: 126 bpm
BP: 130/90 mm Hg
RR: 38 cpm
SPO2: 98% @ RA
SYSTEMIC EXAMINATION:
Patient is examined in a well lit room and in a sitting position.
Upper Respiratory Tract:
Nose: No DNS, polyps, turbinate hypertrophy
Oral cavity: No ulcers
Lower Respiratory Tract:
INSPECTION:
Shape of chest: elliptical
Trachea: appears to be central
Supraclavicular and infraclavicular hollowness absent
Accessory muscles usage - None
Apical impulse Normal
No kyphoscoliosis
No hyperpigmented patches, scars
PALPATION:
All inspectory finding confirmed
Trachea: central
Tactile vocal fremitus: Not assessed
Chest movements: not assessed
PERCUSSION:
Direct: resonant
Indirect: Right Left
Supra clavicular:. Resonant Hyperresonant
Infra clavicular: Resonant Hyperresonant
Mammary: Resonant Hyperresonant
Inframammary Resonant Dull
Axillary: Resonant Hyperresonant
Infra axillary: Resonant Dull
Supra scapular: Resonant Hyperresonant
Infra scapular: Resonant Dull
Inter scapular: Resonant Hyperresonant
AUSCULTATION: Right Left
Supra clavicular:. NVBS NVBS
Infra clavicular: NVBS NVBS
Mammary: NVBS NVBS
Inframammary NVBS Diminished
Axillary: NVBS NVBS
Infra axillary: NVBS Diminished
Supra scapular: NVBS NVBS
Infra scapular: NVBS Diminished
Inter scapular: NVBS NVBS
Pulmonary Area - First and Second Heart Sounds Heard, No other sounds are heard
Aortic Area - First and Second Heart Sounds Heard, No other sounds are heard
PER ABDOMEN:
INSPECTION: Not Distended
PALPATION: Inspectory Findings Confirmed
Soft, non tender
No Organomegaly
PERCUSSION : Tympanic
AUSCULTATION: Bowel sounds Heard
CNS:
No focal neurological deficits
Cranial Nerves intact.
PROVISIONAL DIAGNOSIS:
Left sided HYDRO PNEUMOTHORAX
INVESTIGATIONS:
CT - CHEST
Large non homogenous opacities with air bronchogram and surrounding ground glass opacities is seen in the superior segment of the left lower lobeLIGHTS CRITERIA
- fluid protein/serum protein = 0.22
- fluid LDH/serum LDH = 2.28
- 2/3 of upper limit of serum LDH = 306<513
Exudative Effusion
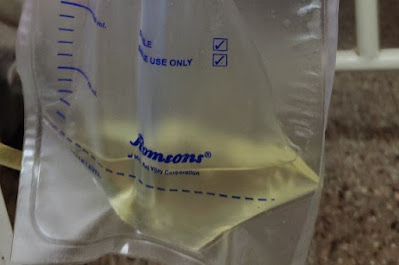
ICD inserted:
Tube: patent
Drain: 200ml
Air column: 3-4cm
Air leak +
Subcutaneous emphysema - Absent
Post procedure vitals:
PR: 128bpm
BP: 120/70mmhg
RR: 36cpm
SPO2: 99% with 12-14 liters/min of oxygen
TREATMENT:
1.O2 inhalation @ 2-3l/min to maintain saturation >94%
2. Inj PIPTAZ 4.5mg IV/TID
3. Inj PAN 40 mg IV/OD/BBF
4. Inj TRAMADOL 1 amp in 100ml NS stat
5. Syrup GRILLINCTUS-DX 2tsp TID
6. Inj ZOFER 4mg IV/STAT
7. T. DOLO 650mg PO BD
8. Monitor vitals- BP, PR, RR, SPO2
9. ICD care:
- Bag always below waist
- Cap always open
- Check air column movement
- Maintain under water seal.
11. Tab. AZEE 500mg PO OD







Comments
Post a Comment